Living with AIH
Patients with autoimmune hepatitis (AIH) typically lead long lives. With treatment, most patients don’t need liver transplants and have normal life expectancies.
Life expectancy.
Patients being treated for AIH do well long-term, and most will never need a liver transplant. In a diverse group of patients (including patients of advanced age), 91% are still living after 10 years, and 70% are still living after 20 years without liver transplants.
Patient stories.
Flare-up symptoms.
Some patients may experience increases in liver tests while on immunosuppression. Patients often refer to these episodes as “flares.” It is not completely clear why flares occur, but some doctors think that either the immunosuppression medication may not have provided excellent control of liver inflammation or a separate condition has caused the increase, such as a viral illness, stress, or another liver condition like fatty liver disease. Patients who don’t take their medication consistently could also increase their risk of a flare.
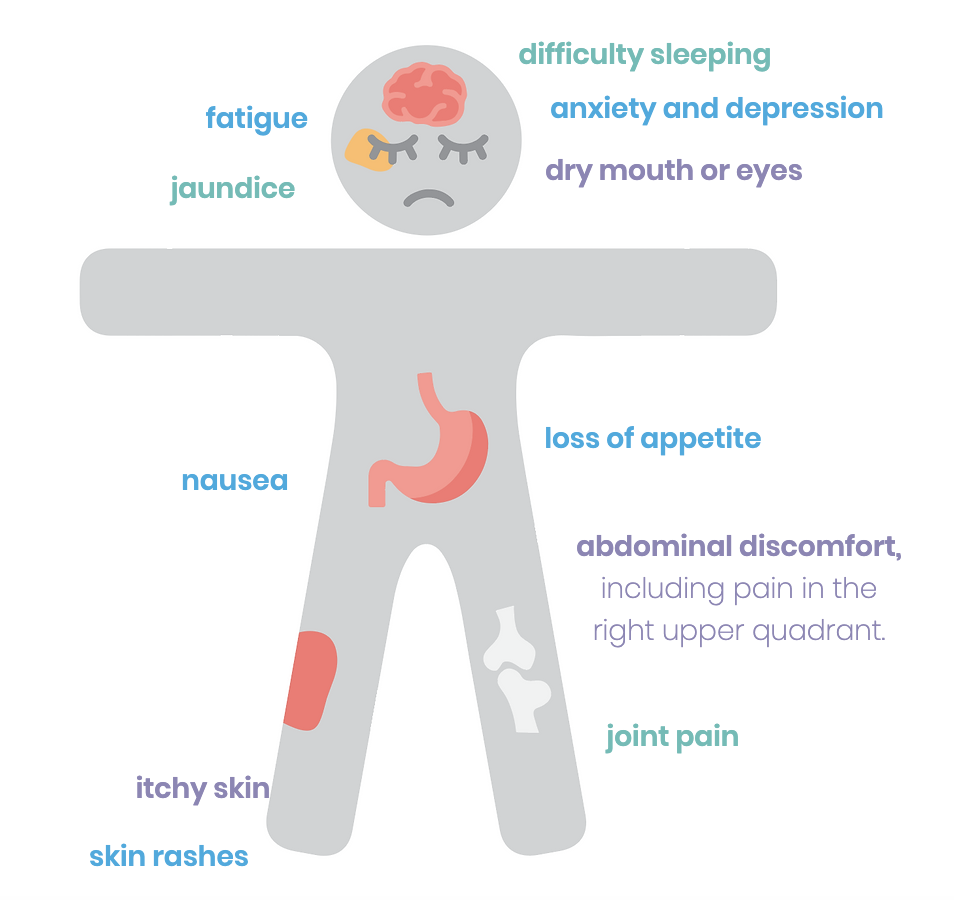
When experiencing a flare, some patients may notice the recurrence of symptoms associated with AIH, such as worsening fatigue, itching, joint pain, and gastrointestinal complaints, among others. Be sure to report any significant changes in your symptoms to your doctor. After a flare, your doctor may prescribe steroid medications again or adjust your long-term immunosuppressant dose or frequency.
Reversing fibrosis.
In some AIH patients whose liver inflammation is well controlled, liver scarring (fibrosis) can be reversed. In small historical studies of AIH patients with follow-up liver biopsies, over 50% of treated patients may see some improvement (reduction) of liver fibrosis.
Improvement in liver fibrosis may also be possible for those with cirrhosis at diagnosis as well. In an early 1990s study, over half of the cirrhotic AIH patients showed improvement of liver fibrosis with treatment. We cautiously interpret these study findings, as large and carefully conducted studies examining this question are still incomplete. There are no good predictors for which patients may have improvement in fibrosis levels with treatment and over what amount of time. Yet, we do know that excellent control of inflammation in the liver is important (normal or low normal liver tests: AST and ALT, as well as IgG).
Often doctors will follow fibrosis levels with the use of noninvasive testing such as FibroScans. Some doctors may order a repeat liver biopsy to track the level of fibrosis and liver inflammation. It is uncommon for doctors to order repeat liver biopsies less than two years apart.
Liver transplants.
Few studies exist showing how many AIH patients need liver transplants. After 10 years of being diagnosed and treated for AIH, about 9 to 10% of patients needed a liver transplant or died from liver-related disease, according to one small study. After 20 years, 30% needed a liver transplant or died from liver-related disease.
Patients with early fibrosis whose liver enzymes return to normal with treatment will likely live long lives without needing a liver transplant or experiencing liver failure.
Take Action.
Become a member of the Autoimmune Hepatitis Association, donate, take part in research opportunities, and find support from people just like you. Sign up for our mailing list for first access to educational content, events, and the latest research!
